
Ryan Nash is a sixteen-year-old sophomore at NAI and on his first year of journalism. His interests include, video games, hiking, and reading. He is also...


January 30, 2020
It’s 4:00 a.m, you can’t sleep. Your meter is reading 487 as you feel your body swelling and a sweat dripping down, you know you need a shot of humalog insulin. But the cost of this once free hormone is too great, so you decide to ration it and just hope your long acting Lantus brings down your blood sugar, trying to fall asleep, not knowing if you will ever wake up.
Insulin, we’ve all heard of this incredible hormone, but for those of us who slept through biology or need a brief reminder, here is what it is: a hormone produced in the pancreas by a specific cell called a ‘Beta-Cell’, or more commonly a ‘B Cell’. This insulin is then used by the body to promote the absorption of carbohydrates, a term for saccharides like starch and sugar that we get from food consumption, from the blood and into organs to control the metabolism of said organs.
Many conditions involve this hormone but there are three that are most often associated with it;
Type 1 Diabetes (alternatively Juvenile Diabetes or diabetes mellitus) is a chronic condition where the body’s immune system attacks the Beta-Cells in the pancreas, stopping the production of insulin. Its nickname ‘Juvenile Diabetes’ comes from the fact that most sufferers are diagnosed with it before the age of 25. There is no prevention for this condition, with treatment involving the injection of insulin (synthetic or extracted from other organisms) to lower blood glucose levels, a component of carbohydrates the body uses. Genetic factors do play a small role but there is a low chance of inheriting it. No other factors have been determined.
Type 2 Diabetes (alternatively Adult-Onset Diabetes) is when the body develops a resistance to the bodies own insulin, due to excess weight and/or insufficient exercise with genetic factors often involved. Its appearance during childhood is very rare, which is why it is called Adult-Onset. Though this condition is chronic, symptoms often vary in severity from one case to another with exercising and a healthy eating style decreasing the severity of it. In some cases, medication and surgery may be an option.
Gestational Diabetes is a big-tent term used describe some women who develop insulin resistance during their 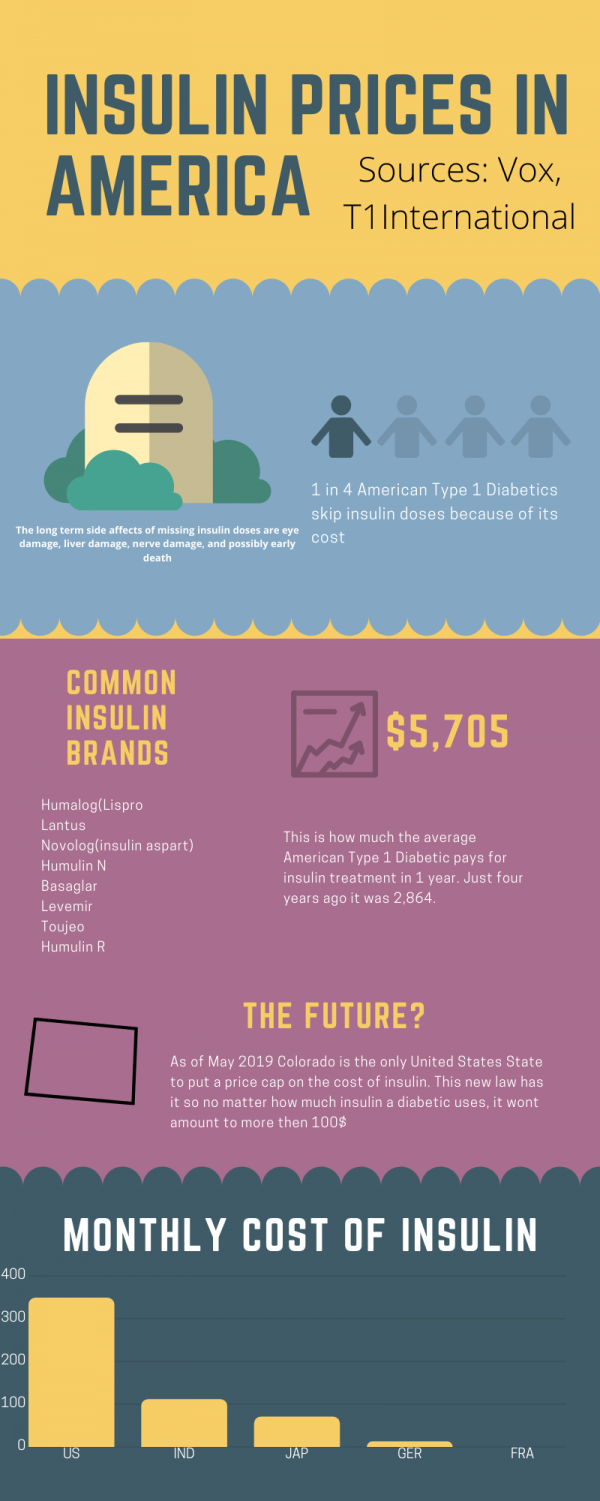 pregnancy. It occurs in roughly 1% of pregnancies where the woman is twenty or younger, with it increasing to 13% of pregnancies by the age of 44. Usually developing during the last three months of a pregnancy, if left untreated it often results in a stillbirth. Risk factors include old age of the woman, overweight, family history of Type 2 Diabetes, being Pacific Islander or Native American, and/or having an abnormal amount of male hormones. Luckily, in 90% of births where the woman has the condition, the symptoms quickly resolve themselves with the mothers insulin resistance and levels returning to normal and a perfectly healthy child. Though the child has a higher chance of developing type 2 diabetes and being overweight later in life, this isn’t set in stone.
pregnancy. It occurs in roughly 1% of pregnancies where the woman is twenty or younger, with it increasing to 13% of pregnancies by the age of 44. Usually developing during the last three months of a pregnancy, if left untreated it often results in a stillbirth. Risk factors include old age of the woman, overweight, family history of Type 2 Diabetes, being Pacific Islander or Native American, and/or having an abnormal amount of male hormones. Luckily, in 90% of births where the woman has the condition, the symptoms quickly resolve themselves with the mothers insulin resistance and levels returning to normal and a perfectly healthy child. Though the child has a higher chance of developing type 2 diabetes and being overweight later in life, this isn’t set in stone.
All three of these conditions are treated with either extracted insulin from animals or the more modern method of artificial production in labs. The only treatment for Type 1 Diabetes is through the injection of insulin necessary for survival, though diet changes and exercise may help manage symptoms. Conversely, for those with Gestational Diabetes and Type 2 Diabetes insulin is also sometimes used. Therefore, insulin injections are a very important tool for the well being and survival millions globally. Yet many are forced to ration (and in some cases go without it for a meal or two) this salient hormone because of its price.
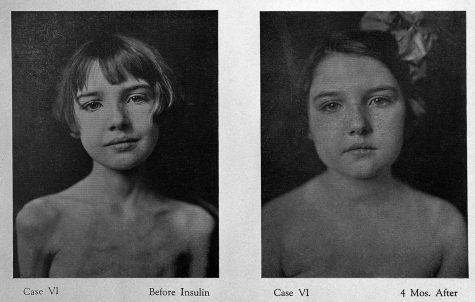
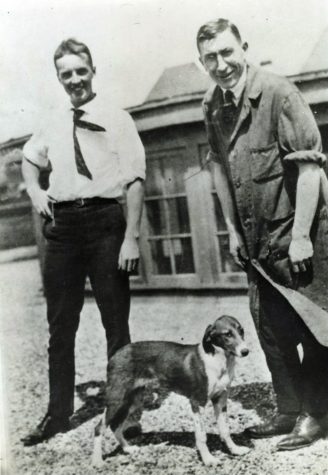
Insulin as a bodily fluid was first described in the 6th BCE century in Egypt and Greece at roughly the same time, but what it did in the body was unknown. In the early part of the 20th century Type 1 Diabetes was first identified with the first treatment being a ‘starvation diet’, a strictly limited diet often being just bird seed. Though this did extend the life of children with it, they were in much pain and would eventually die. In 1921 and 1922 a breakthrough was reached. A surgeon by the name of Frederick Banting studying isolating pancreatic extracts approached John Macleod a professor of physiology at the University of Toronto, who gave him more equipment, space to work, and ten dogs to continue these studies. In late 1921 Dr. Banting and two students named Charles Best and Clark Noble successfully lowered a depancreasised(removal of the pancreas) dog’s blood glucose level by using an extract, they called Isletin, from another dog’s pancreas. Soon the biochemist J.B Collip joined the group to help make this substance usable for humans. On the day of January 11th, 1922 a 14 year old diabetic boy by the name of Leonard Thompson was injected with this Isletin. Initially he suffered an allergic reaction to the substance and an abscess formed were the insulin was injected, but after a sample of his blood was taken and his blood glucose level had increased! This would be the first time a diabetic would be treated with insulin. Not only that but the patent for insulin would be given out for free. Banting and Macleod would win the nobel peace prize in Medicine in 1923, with Banting splitting his prize money with Best, and Macleod splitting his prize money with James Collip. Frederick Banting would also be knighted for his discovery in 1934.
As a side note a Romanian chemist named Nicolae Paulescu may have identified what insulin’s function is in 1916, but wouldn’t publish his findings until 1921 as he was drafted into the Romanian army soon after his discovery. It remains a point of contention if the nobel prize winners in the previous paragraph knew about this or not.
Today, Banting and his co-inventors would be furious at the cost of insulin. They strongly believed that insulin was a right for those who required it no matter their economic situation, but despite what they morally believe many companies and insulin manufacturers don’t follow this philosophy. The average American Diabetic pays $450 monthly for their Insulin, with it somewhat dependent on the specific brand. Yes, I said brand. Today three private companies produce 90% of insulin with many different formulas for insulin, its now produced artificially, that each act slightly differently as some work better than others for some people. Not only this, but one out of every four Americans with diabetes skips doses of insulin because of its cost! Determining the cost of insulin from country to country is quite hard with mixed information existing because of different names for the same kind of insulin but as an example the cost of a humalog brand vial, roughly one month of insulin, is 32$ in Canada and in The United States its about 300$.
How to resolve this varies, from nationalising healthcare to promoting innovation in the industry but many would agree something needs to be done.

Ryan Nash is a sixteen-year-old sophomore at NAI and on his first year of journalism. His interests include, video games, hiking, and reading. He is also...